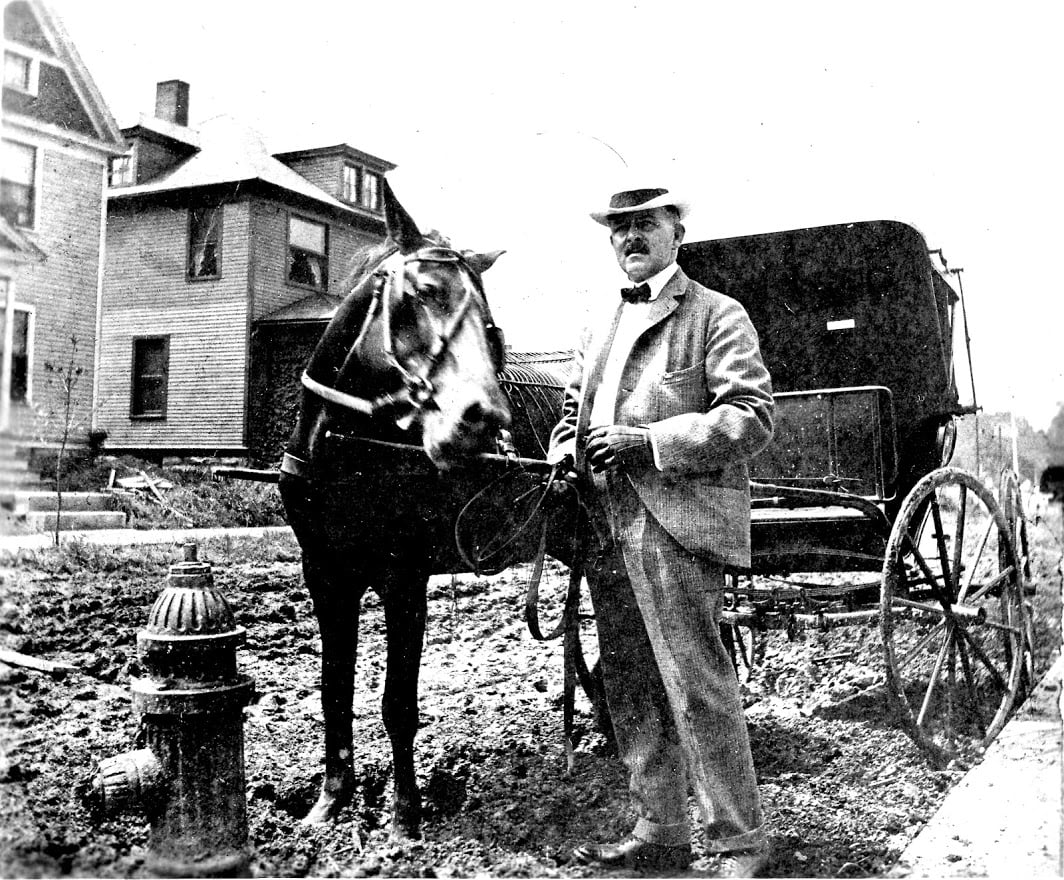
I used to think that only old people reminisced longingly for things to be the way they were in the past! Then I caught myself (and I'm not old!) wistfully watching reruns of westerns and thinking "Gone are the days of Doctors riding mules with black bags to do house calls. But why?"
Have we become so enamored with technology, and all the great modern medical advancements that we've lost sight of the personal touch?
Don't get me wrong - I LOVE MY TECH!! But, no longer do doctors intimately know their patients, their families, their socio-economic situation, their religious beliefs, their goals, dreams, and aspirations.
Is that even a problem? If so, who is gong to fill the gap?
Case Managers!
Now, a question for you - What's your self-funded health plan doing to make those Case Managers available to your health plan members?
No one has a more vested interest in your health plan members getting the right care, at the right time, in the right place, and for the right price than you do.
Let’s imagine a scenario: Jack needs knee replacement surgery in both knees.
What the orthopedic surgeon sees: 64 year old male privately insured patient needing bilateral knee replacement surgery. Oh, and he has diabetes (as an afterthought).
What a savvy orthopedic surgeon sees: 64 year old privately insured patient needing bilateral knee replacement surgery, who also has diabetes, who is likely to retire and go on medicare soon (better hurry up and get those knees done at the higher reimbursement rate under the private insurance).
What a case manager sees: 64 year old actively at work male Jehovah’s Witness patient originally from Latin America who works in maintenance and lives alone on the third floor of an apartment building with no elevator and has had problems with diabetic foot ulcers in the not so distant past that needs total knee replacement surgery on both knees and was referred by his primary care doctor to an orthopedic surgeon.
Just for fun, let’s take this a step further and explore a few of the thousands of things bouncing around in that Case Manager’s head:
Should this patient get this surgery right now? Is his diabetes well controlled enough? Would it be cheaper for him to wait until he retires and goes on Medicare (would his out of pocket there be lower than with his private insurance)? Will that orthopedic surgeon even accept Medicare patients? How did he end up with this Orthopedic surgeon anyway – is he/she in the patient’s PPO network? How experienced is this surgeon? Is he/she board certified? What the infection rate, morbidity/mortality rate at that hospital where the surgery is going to happen? Is this patient potentially going to need blood for this surgery – does the doctor even know he’s a Jehovah’s Witness and will refuse blood, have they put that in his chart? What Spanish language patient education materials can I share with this patient? Who is going to get this patient back and forth to therapy? Wait, how’s this even going to work? He can’t go home after this surgery, he won’t be able to make it up that many steps! Who are the in network rehab providers available? Will rehab require precert under his plan? Is he even willing to go to the in network rehab? Will they have a bed available when he’s ready to transfer? And on, and on, and on!!
Now, your next question could be “but why is it my self-funded health plan’s responsibility to make sure this patient gets Case Management?”
And my answer: “because you’re paying for Jack’s total knee replacements - his surgery, his hospitalization afterward, his rehabilitation, his complications if things go wrong, and you want Jack back to work pronto!”
Did you know that according to AHRQs HCUPnet project, in 2013 a 64 year old privately insured patient getting ONE knee replacement resulted in $55,059 in hospital charges? That is just the hospitalization. That does NOT include the rehab and post-hospitalization services! And it also tells us that 6 out of every 1000 patients ages 45-64 who have ONE knee replacement die while hospitalized.
Did you know that it’s very common in the medical management industry for knee replacement surgery to NOT prompt medical management to initiate Case Management services?
Hopefully by now you're aware of the price gouging that can occur on orthopedic hardware, and that medical management (in conjunction with your claims administrator) needs to take an active role in preventing it (or at least responding to it when it does occur).
AND I haven’t even brought up the fact that domestic travel for total knee replacement just might be an excellent way for the self-funded health plan to control costs better than just relying on the PPO discount…your medical management vendor should be not just Case Managing this patient, but consulting back to you as a plan about options like this. Then implementing special medical management administration when you move forward with those cutting-edge solutions.
Do you see why high-touch medical management is important? Do you see why ongoing medical management consultation back to your plan is so important?

Deborah Ault, RN, CCM, CCP, AATMC, MBA - Deborah has been a Registered Nurse for over 29 years (lovingly referred to as "Nurse Deb"). Before getting into Care Management, her bedside nursing experience included ER, ICU, Doctor's Office, Home Health, and Telephone Triage. Now she is the President of Ault International Medical Management (aka AIMM). Her team of Nurses and Doctors help the right patients to make sure that they are getting the right care, at the right time, in the right place, for the right reason, at the right price, with the right documentation, and generating the right outcome. This is done by ensuring that patients have all the information and tools they need to help them be as healthy & happy as possible as quickly as possible. AIMM also helps patients to navigate the insurance system.